Below are NCLEX Practice Test: Prioritization, Delegation, and Assignment on Renal and Urinary
The Rationale can be found at the end of the last question. You can also check the answer of each question by clicking “Check answer” and you’ll be redirected to the section of this post where the answer can be found. Then, just click “Go back to question”.
I suggest you answer all the questions first to get the real feel of an NCLEX practice test.
![nclex practice test]()
Questions
1. You are providing nursing care for a 24-year-old female patient admitted to the unit with a diagnosis of cystitis. Which intervention should you delegate to the nursing assistant?
a. Show the patient how to secure a clean-catch urine sample
b. Check the patient’s urine for color, odor, and sediment.
c. Review the nursing care plan and add nursing interventions.
d. Provide the patient with a clean-catch urine sample container.
Check answer
2.Which laboratory result is of most concern to you for the adult patient with cystitis?
a. Serum WBC 9000/mm3
b. Urinalysis with 1- 2 WBCs present
c. Urine bacteria 100,000 colonies/mL
d. Serum hematocrit 36%
Check answer
3.
As charge nurse, which of the following patient’s nursing care would you assign to the LPN/LVN, working under the supervision of an RN?
a. A 48-year-old patient with cystitis who is taking oral antibiotics
b. A 64-year-old patient with kidney stones and a new order for lithotripsy
c. A 72-year-old patient with urinary incontinence needing bladder training
d. A 52-year-old patient with pyelonephritis and severe acute flank pain
Check answer
4.
You are admitting a 66-year-old male patient suspected of having a urinary tract infection. Which piece of the patient’s medical history supports this diagnosis?
a. The patient’s wife had a urinary tract infection 1 month ago.
b. The patient has been followed for a prostate disease for 2 years.
c. The patient had intermittent catheterization 6 months ago.
d. The patient had a kidney stone removed 1 year ago.
Check answer
5.
The patient’s admission diagnosis is rule out interstitial cystitis. Based on anticipated physician’s orders, what must your plan of care for this patient include?
a. Daily urine samples fro urinalysis
b. Accurate intake and output records
c. Admission urine sample for electrolytes
d. Teaching about the cystoscopy procedure
Check answer
6.
You are supervising a new graduate RN who is orienting to the unit. The new RN asks why the patient with uncomplicated cystitis is being discharged with orders for ciprofloxacin 250 mg twice a day for only 3 days. What is your best response?
a. “We should check with the physician as the patient should take this drug for 10 to 14 days.”
b. “A 3-day course of ciprofloxacin is not the appropriate treatment for a patient with uncomplicated cystitis.”
c. “Research has shown that with a 3-day course of ciprofloxacin, there is increased patient adherence to the plan of care.”
d. “Longer courses of antibiotic therapy are required for hospitalized patients to prevent nosocomial infections.”
Check answer
7.
Under your supervision, a new graduate RN is teaching the 28-year-old married female client with cystitis methods to prevent future urinary tract infections. Which statement by the new nurse requires that you intervene?
a. “You should always drink 1 to 3 liters of fluid everyday.”
b. “Empty your bladder regularly even if you do not feel the urge to urinate.”
c. “Drinking cranberry juice daily may decrease bacteria in your bladder.”
d. “It’s OK to soak in the tub with bubble bath as it will keep you clean.”
Check answer
8.
You are creating a nursing care plan for an elderly patient with incontinence. For which patient will a bladder-training program be an appropriate intervention?
a. The patient with functional incontinence due to mental status changes
b. The patient with stress incontinence due to weakened bladder neck support
c. The patient with urge incontinence and abnormal detrusor muscle contractions
d. The patient with transient incontinence due to inability to get to toileting facilities
Check answer
9.
The patient with incontinence will be taking oxybutynin chloride (Ditropan) 5 mg by mouth three times a day after discharge. Which information would you be sure to teach this patient prior to discharge?
a. “Drink fluids or use hard candy when you experience a dry mouth.”
b. “Be sure to notify your physician if you experience a heart rate of less than 60 per minute.”
c. “If necessary, your physician can increase your dose up to 40 mg per day.”
d. “You should take this medication with meals to avoid stomach ulcers.”
Check answer
10.
You are providing care for a patient with reflex urinary incontinence. Which action is appropriately delegated to the new LPN/LVN?
a. Teach the patient bladder emptying by the Crede method.
b. Demonstrate how to perform intermittent self-catheterization.
c. Discuss the side effects of bethanechol chloride (Urecholine).
d. Reinforce the importance of proper handwashing to prevent infection.
Check answer
11.
The patient has urolithiasis and is passing the stones into the lower urinary tract. What is the priority nursing diagnosis for the patient at this time?
a. Acute Pain
b. Risk for Infection
c. Risk for Injury
d. Fear of Recurrent Stones
Check answer
12.
You are supervising an orienting nurse who is discharging a patient admitted with kidney stones post lithotripsy. Which statement by the nurse requires that you intervene?
a. “You should finish all of your antibiotics to make sure that you don’t get a urinary tract infection.”
b. “Remember to drink at least 3 liters of fluids every day to prevent another stone from forming.”
c. “Report any signs of bruising to your physician immediately as this indicates bleeding.”
d. “You can return to work in 2 days to 6 weeks, depending on what your physician prescribes.”
Check answer
13.
As charge nurse, you must rearrange room assignments to admit a new patient. Which two patients are best suited to be roommates?
a. A 58-year-old patient with urothelial cancer on multiagent chemotherapy
b. A 63-year-old patient with kidney stones who underwent open uteterolithotomy
c. A 24-year-old patient with acute pyelonephritis and severe flank pain
d. A 76-year-old patient with urge incontinence and a urinary tract infection
_____, _____
Check answer
14.
The patient with polycystic disease (PKD) has the nursing diagnosis Constipation related to compression of intestinal tract. Which nursing care action should you delegate to the newly-trained LPN/LVN?
a. Explain how to choose foods that are high in fiber.
b. Explain how to choose foods that promote bowel regularity.
c. Explore patient’s previous bowel problems and bowel routine.
d. Administer docusate 100 mg by mouth twice a day.
Check answer
15.
You are preparing to insert an intermittent catheter into a male patient to assess for post-void residual urine. Place the following steps I correct order.
a. Assist patient to the bathroom and ask him to attempt to void.
b. Retract the foreskin and hold the penis at 60 to 90-degree angle.
c. Open the catheterization kit and put on sterile gloves.
d. Lubricate the catheter and insert it through the meatus of the penis.
e. Position the patient supine in bed or with head slightly elevated.
f. Drain all urine present in the bladder into the container.
g. Cleanse the glans penis starting at the meatus and working outward.
h. Remove the catheter, clean the penis, and measure the amount of urine returned.
_____, _____, _____, _____, _____, _____, _____, _____
Check answer
16.
You are the admission nurse for a patient with nephrotic syndrome. Which assessment finding supports this diagnosis?
a. Edema formation
b. Hypotension
c. Increased urine output
d. Flank pain
Check answer
17.
The patient has been diagnosed with renal cell carcinoma (adenocarcinoma of the kidney). You are orienting a new nurse to the unit, who asks why this patient is not receiving chemotherapy. What is your best response?
a. “The prognosis for this form of cancer is very poor and we will be providing only comfort measures.”
b. “Chemotherapy has been shown to have only limited effectiveness against this type of cancer.”
c. “Research has shown that the most effective means of treating this form of cancer is with radiation therapy.”
d. “Radiofrequency ablation is a minimally invasive procedure that is the way to treat renal cell carcinoma.”
Check answer
18.
You are teaching a patient how best to prevent renal trauma to the right kidney after an injury that required a left nephrectomy. Which of the following points will you include in your teaching plan? (Choose all that apply.)
a. Always wear a seat belt.
b. Avoid all contact sports.
c. Practice safe walking habits.
d. Wear protective clothing to participate in contact sports.
e. Use caution when riding a bicycle.
Check answer
19.
You are providing nursing care for a patient with acute renal failure (ARF) who has a nursing diagnosis of Fluid Volume Excess related to compromised regulatory mechanisms. Which actions should you delegate to the experienced nursing assistant? (Choose all that apply.)
a. Monitor and record vital signs every 4 hours.
b. Weigh patient every morning using standing scale.
c. Administer furosemide (Lasix) 40 mg orally twice a day.
d. Remind patient to save all urine for intake and output record.
e. Listen to breath sounds every 4 hours.
f. Ensure that patient’s urinal is within reach
Check answer
20.
The nursing assistant reports to you that the patient with ARF has had a urine output of 350 mL for the past 24 hours after receiving furosemide 40 mg IV push. The nursing assistant asks you how this can happen. What is your best response?
a. “During the oliguric phase of acute renal failure, patients often do not respond well to either fluid challenges or diuretics.”
b. ‘There must be some sort of error. Someone must have failed to record the urine output.”
c. “The patient with acute renal failure retains sodium and water, counteracting the action of the furosemide.”
d. “The gradual accumulation of nitrogenous waste products results in the retention of water and sodium.”
Check answer
21.
As charge nurse, which patient will you assign to the nurse pulled to your unit from the surgical intensive care units (SICU)?
a. Patient with kidney stoners scheduled for lithotripsy this morning
b. Newly post-operative patient with renal stent placement
c. Newly admitted patient with acute urinary tract infection
d. Patient with chronic renal failure needing teaching on peritoneal dialysis
Check answer
22.
Your patient is receiving IV piggyback doses of gentamicin every 12 hours. What measurement is your priority for monitoring during the period that the patient is receiving this drug?
a. Serum creatinine and BUN
b. Morning weight every day
c. Intake and output every shift
d. Temperature elevation
Check answer
23.
The patient with a diagnosis of ARF had a urine output of 1560 mL for the past 8 hours. The LPN/LVN who is caring for this patient under your supervision asks how a patient with renal failure can have such a large urine output. What is your best response?
a. “The patient’s renal failure was due to hypovolemia and we have administered IV fluids to correct the problem.”
b. “Acute renal failure patients go through a diuretic phase when their kidneys begin to recover and may put out up to 10 L of urine per day.”
c. “With that much urine output, there must have been a mistake made when the patient was diagnosed.”
d. “An increase in urine output like this is an indicator that the patient is entering the recovery phase of acute renal failure.”
Check answer
24.
The patient on the medical-surgical unit with ARF is to begin continuous veno-venous hemofiltration (CVVH) as soon as possible. What is the priority action at this time?
a. Call the charge nurse and transfer the patient to the intensive care unit.
b. Develop a teaching plan for the patient that focuses on CVVH.
c. Assist the patient with morning bath and mouth care prior to transfer.
d. Notify the physician that the patient’s mean arterial pressure is 68 mm Hg.
Check answer
Rationale
1.
ANSWER D
– Providing the equipment that the patient needs to collect the urine sample is within the scope of practice for a nursing assistant. Teaching, planning and assessing all require additional education and skill, which is appropriate to the scope of practice for professional nurses. Focus: Delegation/supervision
Go back to question
2. ANSWER C –
The presence of 100,000 bacterial colonies/mL in urine or the presence of many WBCs and RBCs indicates a urinary tract infection. The WBC count is within normal limits, and the hematocrit is a little low, which may need follow-up. Neither of these results indicates infection. Focus: Prioritization
Go back to question
3. ANSWER A –
The patient with cystitis who is taking oral antibiotics is stable and has predictable outcomes, therefore appropriate to the scope of practice for the LPN/LVN under the supervision of an RN. The patient with the new order for lithotripsy will need teaching about the procedure, which should be accomplished by the RN. The patient in need of bladder training will need the RN to plan this intervention. The patient with flank pain needs careful and skilled assessment by the RN. Focus: Assignment
Go back to question
4. ANSWER B –
Prostate disease increases the risk of urinary tract infections in men. The patient’s wife’s UTI should not affect the patient. The catheter usage and kidney stone timeframes are too distant to cause the UTI stone timeframes are too distant to cause this UTI. Focus: Prioritization
Go back to question
5. ANSWER D –
A cystoscopy is needed to accurately diagnose interstitial cystitis. Urinalysis may show WBCs and RBCs, but no bacteria. The patient will probably need an admission urinalysis, but not daily samples. Intake and output may be assessed, but will not contribute to the diagnosis. Cystitis does not usually affect urine electrolyte levels. Focus: Prioritization
Go back to question
6. ANSWER C –
For uncomplicated cystitis, a 3-day course of antibiotics is an effective treatment, and research has shown that patients are more complaint with shorter antibiotic courses. Seven-day courses of antibiotics are appropriate for complicated cystitis, and 10-14 day courses are prescribed for uncomplicated pyelonephritis. This patient is being discharged and should not be at risk for a nosocomial infection. Focus: Prioritization
Go back to question
7. ANSWER D –
Women should avoid irritating substances such as bubble bath, nylon underwear, and scented toilet tissue to prevent urinary tract infections. Adequate fluid intake, cranberry juice, and regular voiding are all good strategies for preventing urinary tract infections. Focus: Delegation/supervision, prioritization
Go back to question
8. ANSWER C –
As long as they are alert, aware, and able to resist the urge to urinate, patients with urge incontinence can be taught to control their bladder by starting a schedule for voiding, then increasing the intervals between voids. Patients with functional incontinence related to mental status changes or loss of cognitive function will not be able to follow the bladder-training program. The patient with stress incontinence is better treated with exercises such as pelvic floor (Kegel) exercises to strengthen the pelvic floor muscles. Focus: Prioritization
Go back to question
9. ANSWER A –
Oxybutynin chloride (Ditropan) is an anticholinergic agent, which often causes an extremely dry mouth. The maximum dose is 20 mg per day. This drug can cause tachycardia as a side effect, but does not cause bradycardia. Oxybutynin chloride should be taken between meals because food interferes with absorption of the drug. Focus: Prioritization
Go back to question
10. ANSWER D –
Teaching about bladder emptying. Self-catheterization, and medications requires additional knowledge and training and are appropriate to the scope of practice of the RN. The LPN can reinforce information that has already been taught to the patient. Focus: Delegation/supervision
Go back to question
11. ANSWER A –
When patients with urolithiasis pass stones, the stones can cause excruciating pain for up to 24-36 hours. All of the other nursing diagnoses for this patient are accurate; however, at this time, pain is the urgent concern for the patient. Focus: Prioritization
Go back to question
12. ANSWER C –
Bruising is to be expected after lithotripsy. It may be quite extensive and take several weeks to resolve. All of the other statements are accurate for the patient after lithotripsy. Focus: Prioritization
Go back to question
13. ANSWER C and D –
Both patients will need frequent assessments and medications. The patient on chemotherapy and the newly post-operative patient should not be exposed to any infection. Focus: Assignment
Go back to question
14. ANSWER D –
Administering oral medications appropriately is part of the educational program for the LPN/LVN and is within their scope of practice. Teaching and assessing the patient require additional education and skill and are appropriate to the scope of practice for the RN. Focus: Delegation/supervision
Go back to question
15. ANSWER A, E, C, B, G, D, F, H –
Before checking post-void residual, you should ask the patient to void and then position him. Next you open the kit and put o sterile gloves, lubricate and insert the catheter. It is necessary to drain all urine from the bladder to assess the amount of post-void residual the patient has. Finally, the catheter is removed, the penis cleaned, and the urine measured. Focus: Prioritization
Go back to question
16. ANSWER A –
The underlying pathophysiology of nephritic syndrome involves increased Glomerular permeability that allows larger molecules to pass through the membrane into the urine and be removed from the blood. This process causes massive loss of protein, edema formation, and decreased serum albumen levels. Key features include hypertension and renal insufficiency (decreased urine output). Flank pain is seen in patients with acute pyelonephritis. Focus: Prioritization
Go back to question
17. ANSWER B –
Chemotherapy has limited effectiveness against renal cell carcinoma. This form of cancer is usually treated surgically by nephrectomy. Focus: Supervision/prioritization
Go back to question
18. ANSWER A, B, C, E –
A patient with only one kidney should avoid all contact sports and high-risk activities to protect the remaining kidney from injury and
preserve renal function. Protective clothing is not adequate to ensure safety. All of the other points are key to preventing renal trauma. Focus: Prioritization
Go back to question
19. ANSWER A, B, D, F –
Administration of oral medications is appropriate to the scope of practice of the LPN/LVN or RN. Assessment of breath sounds requires additional education and skill development and is most appropriate within the scope of practice of the RN, but may be part of an experienced and competent LPN/LVN’s observations. All other actions are within the educational preparation and scope of practice for the nursing assistant. Focus: Delegation/supervision
Go back to question
20. ANSWER A –
During the oliguric phase of acute renal failure, patients’ urine output is greatly reduced. Fluid boluses and diuretics do not work well. This phase usually lasts from 8 to 15 days. Although there are frequently omissions with regard to recording intake and output, this is probably not the cause of the patient’s decreased urine output. Retention of sodium and water is the rationale for giving furosemide, not the reason that it is ineffective. Nitrogenous wastes build up as a result of the kidney’s inability to perform their elimination function. Focus: Delegation/supervision
Go back to question
21. ANSWER B –
A nurse from SICU is thoroughly familiar with the care of newly post-operative patients. The patient scheduled for lithotripsy may need education about the procedure. The newly admitted patient needs an in-depth admission assessment, and the patient with chronic renal failure needs teaching about peritoneal dialysis. All of these interventions/actions would best be accomplished by an experienced nurse with expertise in the care of patients with renal problems. Focus: Assignment
Go back to question
22. ANSWER A –
Gentamicin can be a highly nephrotoxic substance. Creatinine and BUN should be monitored for elevations indicating possible nephrotoxicity Focus: Prioritization
Go back to question
23. Answer B –
Patients with acute renal failure usually go though a diuretic phase. The diuresis can result in an output of up to 10 L/day of dilute urine. During this phase, it is important to monitor for electrolyte and fluid imbalances. This is followed by the recovery phase. A patient with ARF due to hypovolemia would receive IV fluids to correct the problem; however, this would not necessarily cause the onset of diuresis. Focus: Supervision
Go back to question
24. Answer A –
CVVH is a continuous renal replacement therapy that is prescribed for patients with renal failure who are critically ill and do not tolerate the rapid shifts in fluids and electrolytes that are associated with hemodialysis. A teaching plan is not urgent at this time. Continuous veno-venous therapy does not require a specific mean arterial pressure and utilizes a blood pump to propel blood through the blood tubing circuit. When a patient urgently needs a procedure, morning care does not take priority and may be deferred until later in the day. Focus: Prioritization
The post NCLEX Practice Test: Prioritization, Delegation, and Assignment on Renal and Urinary appeared first on Nurse Germz.
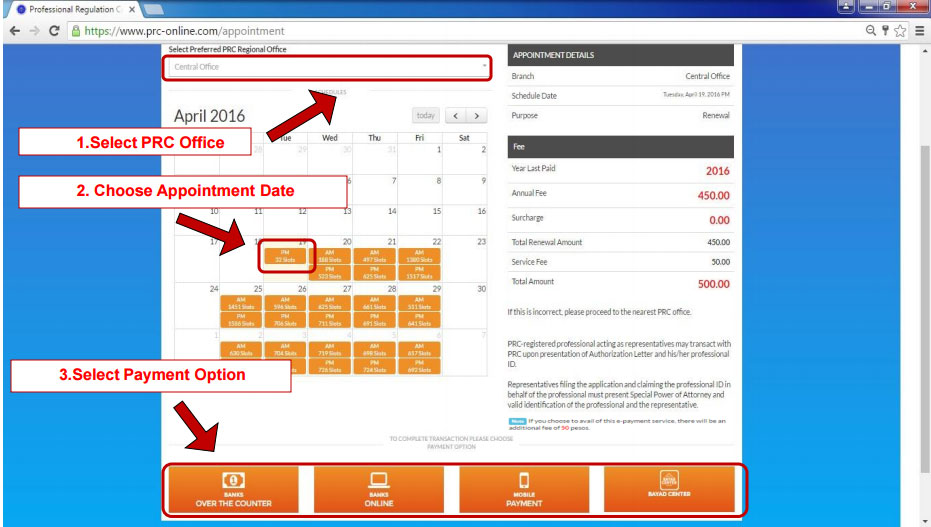
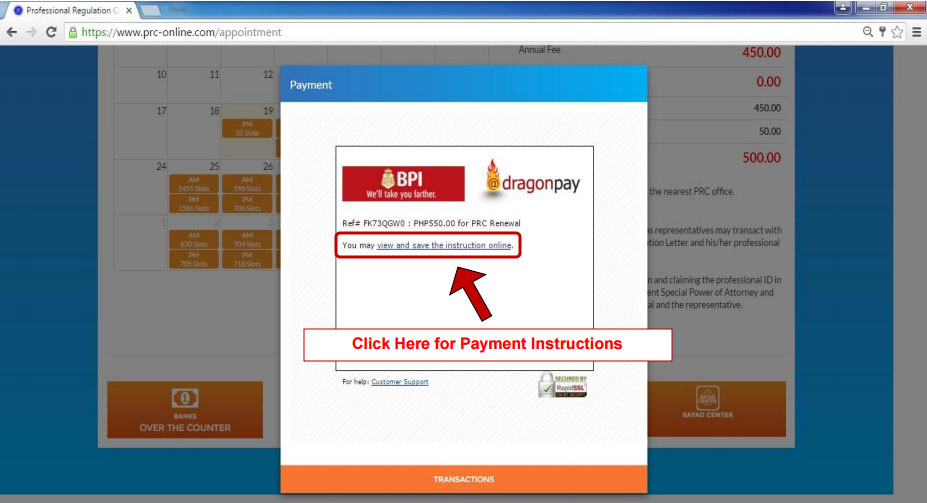
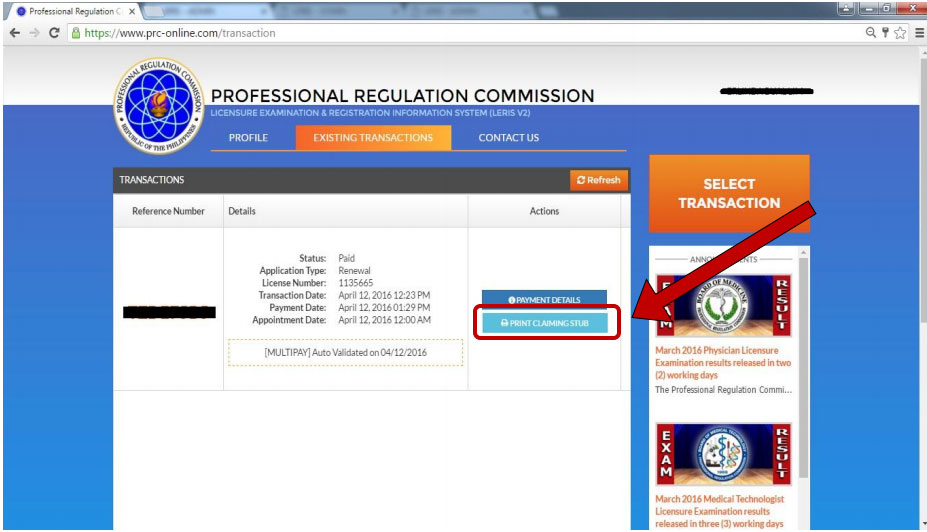
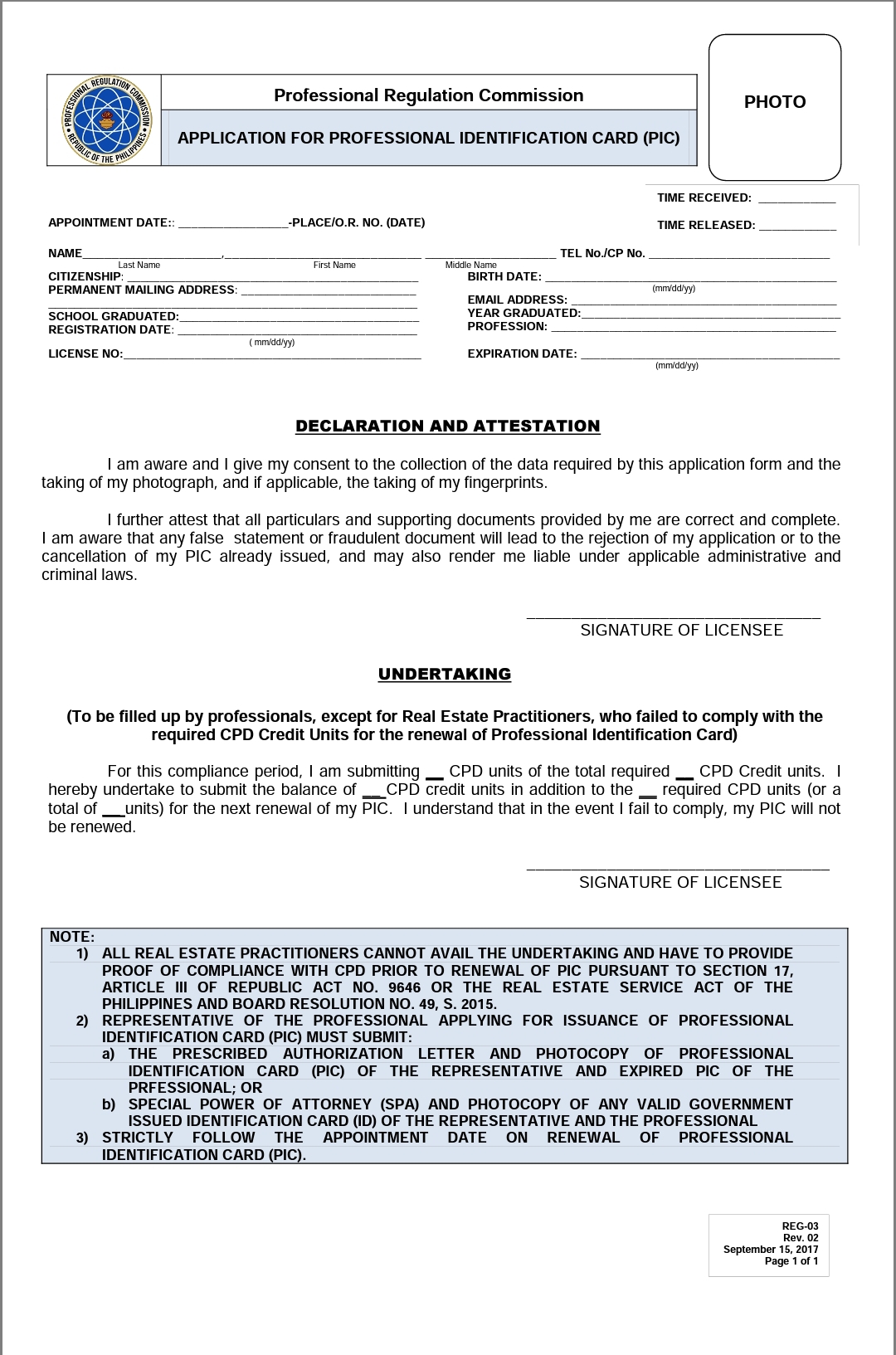
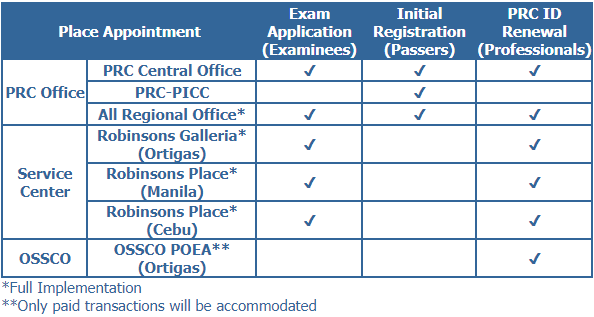
 The Professional Regulation Commission announced yesterday, June 30, 2017 that Professional Registered Nurses are exempted until December 31, 2017 in the compliance with Continuing Professional Development (CPD) required for renewal of Professional Identification Cards.
The Professional Regulation Commission announced yesterday, June 30, 2017 that Professional Registered Nurses are exempted until December 31, 2017 in the compliance with Continuing Professional Development (CPD) required for renewal of Professional Identification Cards.